Last Updated on 30th March 2025 by Charlie Walsh
While most men focus on how well their penis works, its appearance can be just as important for your health. A healthy-looking penis is one of many signs of good overall health. Men with Peyronie’s disease — abnormal curvature of the penis due to scar tissue formation — can have serious cardiovascular, circulatory and thyroid issues, and they may even have an increased risk of certain cancers.
However, a curved penis isn’t always cause for alarm. Just like men themselves, penises come in different shapes, sizes and orientations. There’s no specific degree of curvature that guarantees you have Peyronie’s disease, but there are signs to watch out for, such as a sudden or increasing change in penis shape or orientation.
If you’re worried there might be danger around the bend, read on to find out about the cause, symptoms, diagnosis and available treatment options for Peyronie’s disease.
What Is Peyronie’s Disease?
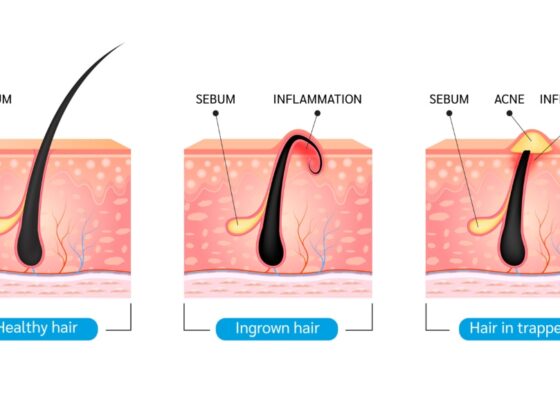
Peyronie’s disease occurs when scar tissue in the penis causes it to abnormally curve, bend or even lose length or girth — potentially from minor injuries to the penis (or penile trauma) sustained during rough sex, sports or another physical activity. Other environmental factors may also play a role in scar tissue formation.
Peyronie’s disease develops in two stages:
- Acute: During this phase is when scar tissue formation noticeably curves or changes the shape of the penis, which can cause pain while erect, flaccid or both. It lasts six months to a year.
- Chronic: At this point, the scar tissue has stopped growing, so there’s no further curvature. However, problems may persist with penis function, like pain during erections and trouble getting or staying hard.
While it’s rare, some men are born with a curved penis, which first becomes noticeable around puberty. If no scar tissue is present, it’s a sign of penile curvature rather than Peyronie’s disease. Scar tissue formation is often prominent enough to feel manually.
Risk Factors Associated With Peyronie’s Disease
There is a range of risk factors that influence your chance of developing Peyronie’s disease:
- Age: Increased risk of abnormal penis curvature is one of several things that happens as you age.
- Autoimmune disorders: Certain autoimmune conditions like lupus can increase your risk.
- Connective tissue disorders: Men with scleroderma, Dupuytren’s disease and other connective tissue disorders are at a greater risk.
- Diabetes: Diabetic men who experience erectile dysfunction (ED) are at significantly greater risk.
- Genetics: If a close male relative (e.g., father or brother) has been diagnosed with Peyronie’s disease, you are at higher risk.
How to Tell If You Have Peyronie’s Disease
Urologists diagnose Peyronie’s disease in about 4% of men between the ages of 40 to 70, but some researchers have come up with higher estimates. Many men feel embarrassed talking about this issue with their doctor, so they put off getting help until serious complications occur or go completely undiagnosed.
The main symptoms of Peyronie’s disease are:
- A bent/curved penis
- Painful lumps on the penis
- Painful erections
- Soft erections
- Chronic penile pain that doesn’t subside
- Difficulty urinating
- Difficulty engaging in sexual intercourse
In most men, scarring (plaques) occurs on top of the penis, causing an upward curve during erections. Likewise, when it occurs on the bottom or side, there is a noticeable curve in those directions. Plaque formation on both sides results in an indented look, and these plaques may even form a ring around the shaft, creating a “bottlenecked” section or hourglass shape.
In extreme cases, the plaques can become calcified and resemble hard bone, which causes intense pain during erections. A man may also notice his penis has gotten shorter or thinner.
When to seek medical assistance
Pay attention to any unusual changes in your penis’ appearance or function, and contact your healthcare provider if these changes become more severe over time. If you’ve already been diagnosed with Peyronie’s disease, consider asking your provider the following questions:
- What should I do if the bend worsens?
- Do you think surgery is necessary?
- When should I return for a checkup?
- Are there any support groups available?
Because Peyronie’s disease can significantly affect your sex life, many men find the diagnosis depressing and even emotionally distressing to communicate to their partner. To help maintain intimacy, don’t be afraid to ask your health care provider for a referral to a qualified sex therapist.
Treatments
In a minority of cases, Peyronie’s disease resolves itself without any treatment. For everyone else, there are a variety of options, including corrective surgery if necessary. And while blades near your penis might sound terrifying, plenty of nonsurgical treatments exist. Here are the major treatment options.
Oral drugs
Your healthcare provider may choose to prescribe oral drugs during the acute phase of your Peyronie’s disease diagnosis. Common choices for oral treatment are vitamin E, carnitine and potassium amino-benzoate. However, studies on their efficacy are mixed.
Vitamin E is a low-cost, low-risk option that doctors typically use for its antioxidant properties, with the goal of shrinking plaques inside the penis. Early studies weren’t well controlled, and the few studies that involve control groups showed no benefit over a placebo.
Carnitine, another antioxidant, is used to help swollen wounds go down. Unfortunately, it had similar results to vitamin E when evaluated with studies using a control group — no better than a placebo.
Potassium amino-benzoate is a B-vitamin complex that has been shown to modestly reduce plaque size, but it won’t fix a penis’ abnormal curvature. It’s also very expensive and can irritate the stomach, so it’s not popular with men in the long term.
Penile injections
Men who fear needles likely aren’t too keen on this option, but injecting high doses of a drug directly into the plaque is more effective than oral treatment. Injections are often requested early in the acute phase by men who want to avoid surgery. The main injectable drugs used for Peyronie’s disease are verapamil, interferon and collagenase.
Verapamil is a calcium-channel blocker often used to treat hypertension, and it may help with pain and bending. Additionally, it’s a low-cost option that’s accessible for most patients.
Interferon is a protein the body makes to control inflammation. It’s used to slow down scar formation, making it a suitable treatment for reducing plaques in Peyronie’s disease patients.
Collagenase is naturally produced by the body and helps break down certain scar tissues. It’s also been proven effective against plaques. In the United States, collagenase injections are approved as a treatment for men with penis curvature that exceeds 30 degrees.
Penile surgery
Though not the most popular, corrective penile surgery is sometimes the last meaningful treatment for Peyronie’s disease. Doctors reserve surgery for men with severe, debilitating cases that make urinating, sitting, sex and other activities difficult. The recommended wait time is nine months to a year after disease progression has stalled.
Doctors perform penile surgery in three basic ways:
- Shortening the side of the penis opposite the plaque
- Lengthening the side of the penis that curves
- Inserting a prosthetic device to fix abnormal curvature and ED
After surgery is over, the patient’s penis is lightly wrapped in a pressure dressing for 24 to 48 hours, and they may be given antibiotics and pain meds. For many men, the next step is guaranteed to be the hardest aspect of recovery — no postsurgical sex for at least six weeks.
Routine Checkups Are Key
Peyronie’s disease can range from a minor nuisance to a devastating, disruptive condition. However, there are good treatment options available, and with the right information and course of action, it’s still possible to have a healthy penis, body and sex life.
Penis health is essential for holistic health, so care for your penis as you would the rest of your body (even if it’s embarrassing). Find a board-certified urologist, get checked out and continue to check in at least once a year. Do that and you’ll be ready for whatever comes around the bend.